|
|
|

Use the ovulation calendar to work out when you will be at your most fertile and able to conceive over the next few months. Click on the above image or the following link to create your own personal fertility calendar
| SEE ALSO | Ovulation Calculator: Charting Fertility |
Vulval itch is the itching of the external vulva or external pubic region in women. It needs to be distinguished from vaginal itching, affecting the internal vagina, although the distinction is sometimes not clear. Vaginal or vulval itching needs prompt professional medical attention and diagnosis.
| LEARN MORE | Vulval itch |
| Unexplained itchy vulva!! |
Documentaire Arte sur le clitoris à travers l’histoire, sa place dans la science. La place du clitoris dans le bien-être de la femme.
Le clitoris ce cher inconnu documentaire ARTE part 1
Le clitoris ce cher inconnu documentaire ARTE part 2
Le clitoris ce cher inconnu documentaire ARTE part 3
Le clitoris ce cher inconnu documentaire ARTE part 4
Le clitoris ce cher inconnu documentaire ARTE part 5
Le clitoris ce cher inconnu documentaire ARTE part 6
Le clitoris ce cher inconnu documentaire ARTE part 7
If you have a persistent itch of the vulva, or any other persistent symptom of the vulva, then see your doctor. It may be a condition called vulval intra-epithelial neoplasia (VIN). This is a skin condition of the vulva. It is not cancer. However, it is classed as a precancerous condition, as in some women, VIN (after several years) may develop into vulval cancer. VIN can affect any woman, but is uncommon under the age of 40. Treatment to clear VIN is usually advised. The aims of treatment include to ease symptoms, and to prevent it developing into vulval cancer.
Neoplasm is an abnormal mass of tissue as a result of neoplasia. Neoplasia (“new growth” in Greek) is the abnormal proliferation of cells. The growth of neoplastic cells exceeds and is not coordinated with that of the normal tissues around it. The growth persists in the same excessive manner even after cessation of the stimuli. It usually causes a lump or tumor. Neoplasms may be benign, pre-malignant (carcinoma in situ) or malignant (cancer).
| LEARN MORE | Vulval Intra-epithelial Neoplasia |
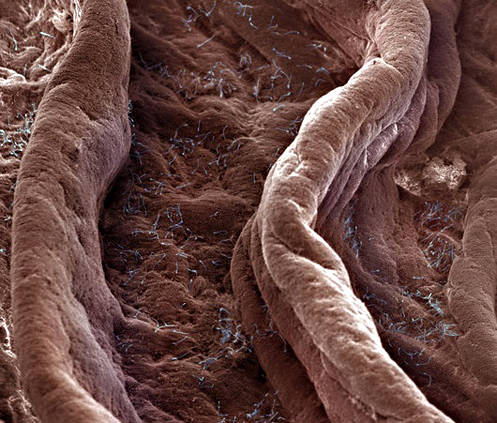
Surface of the human vagina. Magnification: x120 (at 4×4″).
© David Phillips
The vagina (from Latin vagĭna, literally “sheath” or “scabbard”)
Although there is wide anatomical variation, the length of the unaroused vagina of a woman of child-bearing age is approximately 6 to 7.5 cm (2.5 to 3 in) across the anterior wall (front), and 9 cm (3.5 in) long across the posterior wall (rear). During sexual arousal the vagina expands in both length and width. Its elasticity allows it to stretch during sexual intercourse and during birth to offspring. The vagina connects the superficial vulva to the cervix of the deep uterus.
If the woman stands upright, the vaginal tube points in an upward-backward direction and forms an angle of slightly more than 45 degrees with the uterus. The vaginal opening is at the caudal end of the vulva, behind the opening of the urethra. The upper one-fourth of the vagina is separated from the rectum by the rectouterine pouch. Above the vagina is the Mons pubis. The vagina, along with the inside of the vulva, is reddish pink in color, as are most healthy internal mucous membranes in mammals. A series of ridges produced by folding of the wall of the outer third of the vagina is called the vaginal rugae. They are transverse epithelial ridges and their function is to provide the vagina with increased surface area for extension and stretching.
With arousal, the vagina lengthens rapidly to an average of about 4 in.(10 cm), but can continue to lengthen in response to pressure. As the woman becomes fully aroused, the vagina tents (last ²⁄₃) expands in length and width, while the cervix retracts. The walls of the vagina are composed of soft elastic folds of mucous membrane which stretch or contract (with support from pelvic muscles) to the size of the inserted penis or other object, stimulating the penis and helping to cause the male to experience orgasm and ejaculation, thus enabling fertilization.

“Self-Exam” Kit – Includes clear plastic speculum, hand held mirror, small flashlight, lubricant, and “Get the Inside Information” brochure.
Why Cervical/Vaginal Self Exam?
By using a speculum, flashlight and mirror, a woman can observe her own cervix and the natural changes that occur over time. Self exam enables her to see a vital part of her anatomy and monitor changes, secretions, menstrual cycle, and indicators of fertile time. She can identify yeast imbalance, a common vaginal condition. Cervical examination is one of the most powerful tools a woman can have.
Clitoraid is a non-profit organization dedicated to assisting women who have been subjected to genital mutilation practices
Expert instruction for avoiding repeat prolapse after prolapse surgery including essential guidelines after bladder surgery, uterine prolapse surgery and bowel prolapse surgery.
MichelleKenway is a Brisbane, Australia based physiotherapist (physical therapist), author and exercise instructor for women. Her aim is to help women understand and manage their pelvic floor for long term protection and support.
Her website, Pelvic Excercises, is designed to give viewers expert physiotherapy information for great pelvic floor health.









